| |
July 2000
Case of the Month: An 8 year old HIV-infected boy presents with a nontender mass in the right submandibular area. Several weeks later copious amounts of pus spontaneously drain from this lesion.
Answer: Tuberculous lymphadenitis (scrofula)
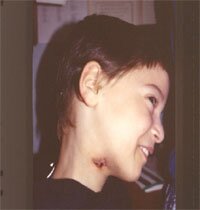 Discussion: Lymphadenitis caused by M. tuberculosis is a relatively rare disease. However, with the advent of HIV, tuberculosis has experienced a resurgence, both as a localized and systemic disease. Of particular concern has been the increase in the frequency of multi-drug resistant disease. In an immunocompromised child other causes of lymphadenitis include infections with gram-positive bacteria, atypical mycobacterium and Bartonella henselae (cat scratch disease); malignancies such as lymphoma; masses such as branchial cleft cysts or cystic hygromas masquerading as lymph nodes; and adenitis due to HIV itself. In contrast with immunocompetent children, HIV-infected children with tuberculous lymphadenitis tend to have multifocal disease with a higher prevalence of systemic spread. The most commonly affected lymph nodes are along the upper border of the sternocleidomastoid muscle. Diagnosis can be made with fine needle aspiration, PCR, acid fast stains, and cultures. If available, ultrasound is useful to detect areas of suppuration. Complete excision is recommended to minimize the potential for fistula formation. Once the diagnosis has been made, treatment with three or four anti-tuberculosis drugs for at least six months is recommended. This regimen typically should include isoniazid, rifampin, and pyrazinamide. Discussion: Lymphadenitis caused by M. tuberculosis is a relatively rare disease. However, with the advent of HIV, tuberculosis has experienced a resurgence, both as a localized and systemic disease. Of particular concern has been the increase in the frequency of multi-drug resistant disease. In an immunocompromised child other causes of lymphadenitis include infections with gram-positive bacteria, atypical mycobacterium and Bartonella henselae (cat scratch disease); malignancies such as lymphoma; masses such as branchial cleft cysts or cystic hygromas masquerading as lymph nodes; and adenitis due to HIV itself. In contrast with immunocompetent children, HIV-infected children with tuberculous lymphadenitis tend to have multifocal disease with a higher prevalence of systemic spread. The most commonly affected lymph nodes are along the upper border of the sternocleidomastoid muscle. Diagnosis can be made with fine needle aspiration, PCR, acid fast stains, and cultures. If available, ultrasound is useful to detect areas of suppuration. Complete excision is recommended to minimize the potential for fistula formation. Once the diagnosis has been made, treatment with three or four anti-tuberculosis drugs for at least six months is recommended. This regimen typically should include isoniazid, rifampin, and pyrazinamide.
|